Greetings All,


Things have been busy enough since I last communicated with the outside world that I have not kept up. …so here’s an update.
The team and the place
Upon arriving at the hospital in an outlying suburb of
The side of the duplex with fewer bedrooms had an expanded kitchen where local ladies prepared us three sumptuous meals a day with abundant local fruit and good coffee. The local tap water is apparently not suitable for
I bunked under Matt Henderson, a
 Matt fights the heebe jeebies seeing first blood assisting Dr Paul Sheldon
Matt fights the heebe jeebies seeing first blood assisting Dr Paul Sheldon
The other bunk in my room was occupied by recently retired orthopedist Ken Freudenberg and his son Nick. Ken is one of Terry’s classmates from med school who lives in
 Ken and Nick do a hand case together
Ken and Nick do a hand case together
Another orthopedist who came is Dr. Paul Sheldon from Victorville, Ca, who has been here several times before. He is young, aggressive, and willing to tackle about anything.
We also have Dennis Madrid a semi-retired anesthesiologist from
 Karen Stagg putting in a spinal
Karen Stagg putting in a spinal
One of the doctors here who got this program started in 1994 is David Mehne, a
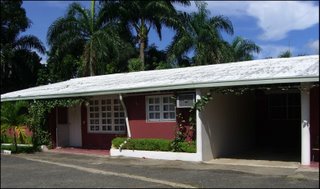
 The street in front of the hospital
The street in front of the hospital
The Work
When this program first started under the auspices of MMI, a medical mission program, (www.MMI.org) they came to an ophthalmologic hospital dedicated to teaching and serving those unable to afford care. There is very little government sponsored medical care here. They first used the ophthalmologic operating rooms, which were not well suited for orthopedics. Eventually another building was built and equipped for orthopedics on the same campus with funds from MMI, a Kiwanis club in the
 Jeannie & Terry Dietrich evaluate a patient
Jeannie & Terry Dietrich evaluate a patient
Terry and David continue to recruit various orthopedic and anesthesia personnel for their two to four times a year trips.
 Karen Stagg with the local nurses
Karen Stagg with the local nurses
The work here consists of seeing patients, who wait lined up in chairs in the hall (the lobby so far is only rebar sticking out of the dirt out front) each morning, and deciding which ones we can help. They hand carry their own x-rays, many of which are poorly exposed and wrinkled from handling, and come NPO, in hopes of getting their surgery done that day. The cases are fascinating and often nothing like what I would see in private practice in the States. Many are horrible late results of old moto accidents. Motos are the ubiquitous moped type motorbikes that they all ride here for basic transportation…often with up to three people and/or seemingly impossible cargo loads, all without helmets. If they have a horrific accident, they are taken to a hospital and put up in traction until the family comes up with enough money to pay for the needed implant; intramedullary rod or plate and screws, etc. If they can’t come up with the several hundred to thousand dollars (usual income here…when they can find employment is a couple hundred a month) in a few days they are put in a plaster cast and sent home to heal as best they can. Some of our patients have not walked since, or can only walk with crutches or walkers, making them unemployable.
Another group of patients are relatively young people with knee injuries. Since no one in this country is trained in arthroscopy, the ability to trim out a bucket handle meniscus tear that has been blocking the patient’s ability to straighten their knee for weeks to years and get them walking and home the same day makes the team here look like miracle workers to the locals. There are also many torn anterior cruciate ligaments…again a moto accident staple injury…that Terry and team can repair. Terry has had a local orthopedist working with him this week, trying to teach him arthroscopy, so he can eventually work here for the indigents when the team is not here.
One of the frustrations of working here is seeing people we know we could help with the proper resources, which we lack. There are several boxes here of interlocking intramedullary nails, a device used to put down the middle of badly broken femurs, tibias, and humerus bones, that are not readily usable because they have no C-arm xray machine. If anyone out there knows of a donateable or inexpensive C-arm, that’s not on its last legs…repair would be a daunting to impossible process here…please let me know.
Some typical deformities...that would do well with I.M. rods
My preconceived notion of my duties here, that I would be doing total joints all day, was mistaken. Because we have Dr Mehne here this trip, he has been doing total hips all day, each day, including very difficult primaries (people with very deformed bones to start with) and revisions (redoing old total hips that have worn out or come apart over time). Total knees have not been too successful here, because of the lack of post op therapy…the patients go home the same day or the next morning…and unsanitary conditions at home. This hospital doesn’t have inpatient beds, just preop and postop wards that we hold a few patients in overnight. There is a relationship with a nearby inpatient facility in case of problems, such as an obese female total hip patient that had to be transferred by ambulance in the middle of the night with a post op pulmonary embolism…she did well.
My duties have been seeing and evaluating patients with an interpreter…my marginal language skills have not come back to me as quickly as I’d hoped. Doing and assisting various surgeries; from simple hardware removals to complex wedge osteotomies (cutting the bone and putting in bone graft from their pelvis and plates and screws to hold it at a more normal angle) for old malunions (healed, but crooked bones).
Our 10 to 14 hour days begin with a delicious breakfast, a hundred yard walk across a little bridge over a lush tropical arroyo to the hospital. The hospital compound is a nicely maintained clean, manicured tropical walled paradise. My one brief excursion across the street to a local grocery for a Coke was a shocking contrast of busy city potholed bustling streets crowded with typical third world shops and street vendors. Behind the hospital, I was told, is a vast ghetto of shacks and mud rutted paths. The gates have full time armed guards, the one near our duplex was packing a pistol grip twelve guage.
 The path and bridge to the hospital
The path and bridge to the hospital
We usually were able to get back to the duplex for lunch and then supper. The ladies who prepared our meals were most accommodating to our straggling in at all hours and in shifts, working around the surgeries at the hospital. The surgeries were scheduled and coordinated as we could based on the availability of rooms (there are four operating rooms), which patients actually showed up that day (they pay a little to no money to the hospital in advance, based on income and some are not able to come up with the cash), which patients were NPO (not eating before surgery is not a universally understood concept), the availability of anesthesia (Dennis worked in the total room with David all day, so we had Karen and most days various local anesthesiologists who came as they could when finished with the ophthalmology cases), and which of our equipment was suitable and currently working.
The ability to innovate here is a necessity. For instance the arthroscopy irrigation system is a wooden platform hung by rope from a pulley hooked to the ceiling supporting a five gallon collapsible water jug containing hospital sterilized water. The rubber tube end is clamped and covered with a sterile latex glove between cases. The power from the hospital’s generator went off several times a day, from a second or two, to up to 10 minutes. After standing in the dark ‘til the power is back, one must reset the anesthesia monitors and the tourniquet pump.
We discovered the last day that a back up battery in the tourniquet pump was shot, so will bring a new one next visit. The generator was found, after we left, to have a clogged oil filter and is now working without interruption.
A couple of highlight cases of the week for me were a tibial osteotomy with vascular complication and the first
The tibial osteotomy was a young man with the upper end of his shin bone (tibia) healed at such an extreme varus (bow legged) angle that he could only walk with crutches. While Paul harvested bone graft from his iliac crest (pelvis) I made the cut in his tibia. We then forced the cut in the bone open to straighten his leg and were about to put in the bone graft and a stainless steel plate and screws to hold it in place when a power outage caused the tourniquet to deflate. There was an inordinate welling up of bright red blood from the back of the knee, indicating a tear in a main vessel, in an area we could not visualize. While we reinflated the tourniquet and finished the graft and hardware placement, then turned the patient over and opened the back of his knee for a vascular repair, people were calling around and found a vascular surgery fellow (not usually found in this country) who was available to come and help us. We found a tear in the anterior tibial branch of the main artery which had been stretched to failure as we straightened his leg by a combination of the patient’s distorted anatomy and scar tissue. We had to tie it off, which could have made the muscles in the front of the leg die, making him unable to actively pull up the front of his foot or toes, but fortunately he had good enough collateral circulation that he had a good dorsalis pedis pulse (the one on the top of the foot) and only some temporary decreased sensation and tingling on the top of his foot which cleared up overnight.
Another exciting case was a patient with a badly worn out lateral (outer side of the knee) compartment, which we were able to fix with the first
 Ken, Karen, Randy, & Terry put in the first Oxford knee in the country
Ken, Karen, Randy, & Terry put in the first Oxford knee in the country
Unfortunately we were not able to do a second similar procedure that had been scheduled because of failure of the batteries for the power equipment and unavailability of anesthesia. We finished the first case with a sterilized Black & Decker drill plugged into the wall socket and Karen had to fly home and none of the local/back up anesthetists were available.
Overall it has been an enlightening and spiritually uplifting experience. The camaraderie and dedication of all the team has been marvelous. The gratitude of the patients and their families warms your heart and makes me want to return over and over.